Medication for pain relief
In a normal, uncomplicated labour and delivery, the use of medication is not always necessary. Your own resources are often enough.
Some labours, however, are exceptionally long, difficult and complicated and the benefits of medication or intervention outweigh the risks. Discuss your alternatives and how they will affect you with your caregiver.
Pain relieving medications fall into two general categories: systemic and regional anaesthesia.
Systemic medication commonly used for labour
- Analgesics, such as pethidine, reduce pain and help relaxation.
- Tranquillisers enhance relaxation, and relieve anxiety.
- Systemic medications enter the bloodstream, affect the whole body and pass
to the baby through the placenta. - Inhalation agents, such as entonox (gas and air), produce a rapid loss of
sensation, and are often used in late first stage of labour.
These medications can be given in one of the following ways:
- Intravenously
- Orally.
- Rectally.
- By injection.
- By inhalation.
The timing of the administration of the drugs in relation to the time of birth will affect the degree of side effects.
Benefits
- May reduce pain, promote relaxation and improve comfort.
- May improve the progress of labour and decrease the pain of surgical intervention.
- May shorten the labour to benefit a distressed baby.
Risks
- Your blood pressure may be affected, causing dizziness, disorientation or loss
of control. - The progress of labour may be slowed down and your urge to push reduced,
which increase your need for further intervention. - May affect the baby by causing an abnormal foetal heart rate, difficulty with
breathing or drowsiness and inhibited sucking reflexes, which could result in a
slow start to breastfeeding.
What is an epidural?
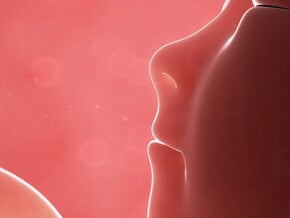
An epidural is a form of regional analgesia or anaesthesia, where a local anaesthetic is injected into the epidural space of the spinal column. This space is filled with fat, nerves and blood vessels and surrounds the entire spinal cord.
The injection numbs the nerves which transmit pain signals from the uterus and birth passage. An epidural is performed under sterile conditions by an anaesthetist or an obstetrician. You will be given an intravenous infusion (drip) prior to the procedure to counteract the drop in blood pressure that occurs with an epidural.
Your doctor or anaesthetist may perform an epidural procedure in the following way:
- A single initial injection of a specific amount of local anaesthetic (not done very often).
- The top-up system, where a local anaesthetic is injected at regular intervals, through an epidural catheter into the epidural space. This must be done by an anaesthetist and cannot be done by ward staff.
- Continuous infusion of a local anaesthetic through an epidural catheter regulated by an infusion pump, of which the rate is determined by the doctor. This method is the most popular. The extent of analgesia/anaesthesia depends largely on the amount of medication used. A mild solution will block small nerve fibres, while a stronger solution blocks the more resistant fibres.
The procedure
You will be required to sign a consent form giving permission for the procedure to be done.
An epidural should only be administered when you are in active labour. An intravenous drip will be inserted before the procedure starts to provide you with the fluid needed to counteract a possible drop in your blood pressure. This protects you and your baby. It also means you have an open vein should you need any emergency drugs. The drip remains in place throughout labour and birth. You will be asked to lie on your side in a curled-up position, or to sit up and lean over so that the vertebrae open up for the insertion of the epidural needle.
The anaesthetist applies a local anaesthetic to the skin where the epidural needle is inserted. This will burn slightly and is probably the last thing you will feel. The epidural needle is placed slowly and carefully between two vertebrae in the lower back at about hip height (anywhere between lumbar vertebrae one and four or higher for a
Caesarean section).
Options to discuss with your doctor
- Systemic medication.
- Nitrous oxide.
- Regional anaesthesia.
- TENS.
If it is administered during labour, it is applied between contractions because you need to keep absolutely still. The anaesthetic is introduced through a catheter into the epidural space. Pain relief starts within about 20 minutes and is usually in full effect after 30–40 minutes.
You will need a catheter to empty your bladder once your feeling has diminished.
You are anaesthetised from your belly button to pelvic region, which includes the vaginal and perineal areas. For a Caesarean, this area is extended to the top of the uterus.
Due to loss of sensation in your legs, you are confined to bed and can no longer move around or position yourself into optimum labour and birth positions. You will be pain-free for approximately four hours, after which a further dose of local anaesthetic may be administered through the epidural catheter.
Mobile epidurals
Advantages of an epidural
- Most effective/superior form of pain relief available.
- Alleviates stress for mother and baby – prevents anxiety and a slow-down in the progression of labour.
- Puts a distressed mother into a smiling, comfortable state by being spared the full force of the contractions.
- Dampens contractions or totally abolishes the pain, making labour more tolerable.
- Saves energy for the ‘power hour’, when all the mother’s reserves are needed for pushing.
- A good, effective epidural means the mother is fully aware, relaxed and participating.
- Lowers high blood pressure due to stress, tension and anxiety.
- The level of analgesia can be controlled easily.
- Has very little effect on the baby.
Transcutaneous Electrical Nerve Stimulation (TENS)
TENS is a fairly new method of pain relief, but not yet widely available in Southern Africa. Small amounts of electrical current (controlled by the mother) stimulate your body to increase the production of natural painkillers (endorphins). Procedure
- Electrodes are taped to the back and connected by wires to a battery-operated obstetric pulsar.
- The pulsar is operated by the mother to give small intermittent safe amounts of current.
Benefits
- Self-controlled as mother remains conscious.
- No drugs and no known side-effects to mother or baby.
- Freedom of movement throughout labour.
- Some pain relief.
- May be removed at own discretion if disliked.
Risks/Disadvantages
- No guaranteed pain relief.
- Cannot be used with pacemakers.
- Not always available.
- May be irritating.
- Cannot be used in a bath or pool.
- Needs to be implemented or practised before labour begins.
Note: A similar effect to TENS can be achieved with small (0,5 ml) injections of sterile water into the skin at the sites where pain is experienced (producing a stinging sensation).
Consult the following sources for more information:
- Caregiver.
- Childbirth educator.
- Childbirth associations.
Risks of an epidural
- Not suitable for a homebirth, as it has to be done in a hospital setting.
- Not suitable for a waterbirth.
- Mother is more likely to spend most of her labour in bed and thus will not be able to take advantage of gravity or upright weight-bearing positions, which help the pelvis to fully open up.
- Takes half an hour to prepare and administer.
- It is a delicate procedure that can only be done by a highly skilled person.
- Lowered blood pressure may reduce blood flow to the placenta and baby, causing distress and an irregular heartbeat.
- There is always the risk of a reaction to the drugs – a test dose is usually given before the actual procedure. Side effects include itching and shivering.
- The mother may experience a loss of control over a very powerful experience.
- Increased risks of intervention with synthetic hormones to keep labour going.
- The use of forceps to pull the baby out if the mother cannot push effectively, and possibly the need for a Caesarean if labour becomes long and drawn out.
Potential long-term risks
- Headache In fewer than one in a hundred women, the epidural needle may pierce the membrane surrounding the spinal fluid and cord. This can cause a severe, blinding headache (post-spinal headache), which is relieved by lying flat, but recurs when sitting up and may last a few days. Notify your caregiver, if the headaches do not go away. The condition can be treated very effectively.
- Backache The effect of the anaesthetic can unwittingly strain the large back muscles, which can go unnoticed until the anaesthetic wears off. This may lead to backache after the birth. Recent research has shown, however, that there is no scientific association between chronic backache and epidurals.
- Less than 10% of epidurals are ineffective. Should pain relief occur on one side of your abdomen and not the other, the anaesthetist will immediately reposition the catheter.
What is a spinal block?
A spinal block is the procedure of choice for a woman about to undergo a Caesarean section. The procedure is identical to that of an epidural with regard to its positioning, but the drug is injected directly into the spinal fluid (instead of the epidural space) and there is no residual catheter.
The advantage is that the drug acts immediately and offers a more reliable form of anaesthesia, unlike the epidural where patchy areas of pain may occur. The effect of the drugs given through the spinal route lasts about one-and-a-half hours as opposed to the four hours from an epidural.
Some anaesthetists combine spinal and epidural anaesthesia to provide the mother with the quick action and reliability of the spinal, as well as the longer lasting effects of the epidural, and the ability to top up the epidural when necessary.
Regional anaesthesia
This is a local anaesthetic given by injection, producing numbness in the area injected or in the part of the body which is supplied by the affected nerves (a nerve block).
- Epidural and spinal anaesthesia.
- Local anaesthetic in perineum.
Benefits
- Relieves pain during active labour and birth.
- Blocks pain impulses.
- Does not cause drowsiness or affect your state of mind.
Risks
Risks vary, depending on the area injected, anaesthesia and dosage.
- Your blood pressure may be lowered, your bearing-down reflex inhibited, and you may experience a post-spinal headache.
- Anaesthetics in the baby’s blood stream may change the heart rate, suppress body functions and alter the neurological behaviour during the baby’s ‘newborn’ period.
- The baby may be affected indirectly by your response to the anaesthetic.